Rol de la función mitocondrial en el corazón y sus implicaciones en disfunciones cardíacas
Main Article Content
Keywords
Mitocondria, mitocondria, función cardíaca, falla cardiaca, falla cardíaca, disfunciones mitocondriales
Resumen
En este artículo de revisión, examinamos el papel de la mitocondria en el buen funcionamiento del corazón, y en la generación de diversas afecciones cardíacas, las cuales están caracterizadas por una baja producción
de energía por parte de las mitocondrias y, por ende, hay un aumento en la pérdida de cardiomiocitos que conlleva al mal funcionamiento del corazón. Se ha determinado, que ciertas disfunciones mitocondriales asociadas a trastornos cardíacos se relacionan con alteraciones del sistema de fosforilación oxidativa, así como, con la disminución de ciertos componentes estructurales como la cardiolipina y la formación de supercomplejos. Se estima que cerca del 2.3% de la población colombiana puede presentar una prevalencia a la falla cardíaca. La presente revisión tiene como objetivo dar a conocer los avances investigativos relacionados con enfermedades cardíacas ocasionadas por disfunción mitocondrial, así como, la identificación de diferentes investigaciones dirigidas en la creación de alternativas de tratamiento para dichas patologías, todo esto con el fin de contribuir a la construcción de líneas de trabajo que tomen a la mitocondria como blanco terapéutico.
Descargas
Referencias
[2] J. Marín-García, A. Akhmedov, and G. W. Moe, “Introduction to Mitochondria in the Heart,” Mitochondria and Their Role in Cardiovascular Disease, vol. 1, pp. 3–9, 2013.
[3] C. H. Babette and B. G. Asa, “Mitochondrial quality control in the myocardium: Cooperation between protein degradation and mitophagy,” Journal of Molecular and Cellular Cardiology, vol. 75, pp. 122–130, 2014.
[4] C. R. Ventura, A. Garnier, V. Veksler, and F. Joubert, “Bioenergetics of the failing heart,” Biochimica et Biophysica Acta-Molecular Cell Research, vol. 1813, pp. 1360–1372, 2011.
[5] M. Rosca, I. Okerec, N. Sharmac, W. Stanley, F. Recchiae, and C. Hoppela, “Altered expression of the adenine nucleotide translocase isoforms and decreased ATP synthase activity in skeletal muscle mitochondria in heart failure,” Journal of Molecular and Cellular Cardiology, vol. 46, pp. 927–935, 2009.
[6] M. Rosca, B. Tandler, and C. Hoppel, “Mitochondria in cardiac hypertrophy and heart failure,” Journal of Molecular and Cellular Cardiology, vol. 55, pp. 31–41, 2013.
[7] E. Griffiths, I. Friehs, E. Scherr,D. Poutias, F. McGowan,and P. Nido, “Electron transport chain dysfunction in neonatal pressure-overload hypertrophy precedescardiomyocyteapoptosisindependent ofoxidativestress,” The Journal of Thoracic and Cardiovascular Surgery, vol. 139, pp. 1609–1617, 2009.
[8] A. L. Andreu, N. Checcarelli, S. Iwata, S. Shanske, and S. Dimauro, “A Missense Mutation in the Mitochondrial Cytochrome b Gene in a Revisited Case with Histiocytoid Cardiomyopathy,” Pediatric Research, vol. 48, pp. 311–314, 2000.
[9] C. S. Kadambari, L. Ling, D. Erinne, W. Xua, R. Ribeiro, P. A. Hecker, F. A. Recchia, R. Sadygov, B. Willard, T. Kasumov, and W. Stanley, “Cardiac mitochondrial proteome dynamics with heavy water reveals stable rate of mitochondrial protein synthesis in heart failure despite decline in mitochondrial oxidative capacity,” Journal of Molecular and Cellular Cardiology, vol. 75, pp. 88–97, 2014.
[10] A. Gvozdjáková, “Chapter 1: Mitochondrial Physiology,” Mitochondrial Medicine, vol. 1, pp. 1–17, 2008.
[11] T. Mercer, S. Neph, M. Dinger, J. Crawford, M. Smith, A. Shearwood, E. Haugen, C. Bracken, O. Rackham, J. Stamatoyannopoulos, A. Filipovska, and J. Mattick, “The Human Mitochondrial Transcriptome,” Cell, vol. 146, pp. 645–658, 2011.
[12] S. Vakrou and R. Abraham, “Hypertrophic cardiomyopathy: a heart in need of an energy bar?” Journal of Frontiers in Physiology, vol. 5, pp. 1–8, 2014.
[13] Y. Ikeda, S. Sciarretta, N. Nagarajan, S. Rubattu, M. Volpe, G. Frati, and J. Sadoshima, “New Insights into the Role of Mitochondrial Dynamics and Autophagy during Oxidative Stress and Aging in the Heart,” Journal of Oxidative Medicine and Cellular Longevity, vol. 1, pp. 1–13, 2014.
[14] U. A. Mukherjee, S. B. Ong, S. G. Ong, and D. J. Hausenloy, “Parkinson’s disease proteins: Novel mitochondrial targets for cardioprotection,” Pharmacology & Therapeutics, vol. 156, pp. 34–43, 2015.
[15] C. Vasquez-Trincado, I. García Carvajal, C. Pennanen, V. Parra, J. A. Hill, B. A. Rothermel, and S. Lavandero, “Mitochondrial dynamics, mitophagy and cardiovascular disease,” The Journal of Physiology, vol. 594, pp. 509– 525, 2016.
[16] L. Chen, Q. Gong, J. P. Stice, and A. A. Knowlton, “Mitochondrial OPA1, apoptosis, and heart failure,” Cardiovascular Research, vol. 84, pp. 91–9, 2009.
[17] F. Billia, L. Haucka, F. Konecnyc, V. Raod, J. Shene, and T. W. Maka, “PTEN-inducible kinase 1 (PINK1)/Park6 is indispensable for normal heart function,” Proceedings of the National Academy of Sciences, vol. 108, pp. 9572–9577, 2011.
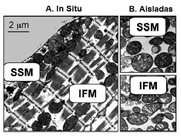
[18] E. L. Holmuhamedov, A. Oberlin, K. Short, A. Terzic, and A. Jahangir, “Cardiac Subsarcolemmal and Interfibrillar Mitochondria Display Distinct Responsiveness to Protection by Diazoxide,” Journal of PLOS ONE, vol. 7, pp. 1–7, 2012.
[19] T. Kasumov, E. R. Dabkowski, K. C. Shekar, L. Li, R. F. Ribeiro, K. Walsh, S. F. Previs, R. G. Sadygov, B. Willard, and W. C. Stanley, “Assessment of cardiac proteome dynamics with heavy water: slower protein synthesis rates in interfibrillar than subsarcolemmal mitochondria,” The American Journal of Physiology-Heart and Circulatory Physiology, vol. 304, pp. H1201–H1214, 2013.
[20] R. Ferreira, R. Vitorino, R. M. Alves, H. J. Appell, S. K. Powers, J. A. Duarte, and F. Amado, “Subsarcolemmal and intermyofibrillar mitochondria proteome differences disclose functional specializations in skeletal muscle,” Journal of Proteomic, vol. 10, pp. 3142–3154, 2010.
[21] J. W. Palmer, B. Tandler, and C. L. Hoppel, “Biochemical Properties of Subsarcolemmal and Interfibrillar Mitochondria Isolated from Rat Cardiac Muscle,” The Journal of Biological Chemistry, vol. 252, pp. 8731–8739,1977.
[22] M. G. Rosca, E. J. Vazquez, J. Kern, W. Parland, M. Chandler, W. Stanley, H. Sabbah, and C. L. Hoppel, “Cardiac mitochondria in heart failure: decrease in respirasomesand oxidative phosphorylation,” Journal of Cardiovascular Research, vol. 80, pp. 30–39, 2008.
[23] T. L. Croston, D. Thapa, A. A. Holden, K. J. Tveter, S. E. Lewis, D. L. Shepherd, C. E. Nichols, D. M. Long, M. Olfert, R. Jagannathan, and J. Hollander, “Functional deficiencies of subsarcolemmal mitochondria in the type 2 diabetic human heart,” The American Journal of Physiology-Heart and Circulatory Physiology, vol. 307, pp. H54–H65, 2014.
[24] B. Chance and G. R. Williams, “Respiratiry Enzymes in Oxidative Phosphorylation - Yhe Steady State,” The journal of Biological Chemistry, vol. 1, pp. 409–427, 1955.
[25] J. Duan and M. Karmazyn, “Effect of verapamil on phosphate-induced changes in oxidative phosphorylation and atractyloside-senitive adenine nucleotide translocase activity in two populations of rat heart mitochondria,” Biochemical Pharmacology, vol. 38, pp. 3873–3878, 1989.
[26] J. S. Monette, L. A. Gómez, R. F. Moreau, B. A. Bemer, A. W. Taylor, and T. M. Hagen, “Characteristics of the rat cardiac sphingolipid pool in two mitochondrial subpopulations,” Biochemical and Biophysical Research Communications, vol. 398, pp. 272–277, 2010.
[27] S. Cogliati, J. A. Enriquez, and L. Scorrano, “Mitochondrial Cristae: Where Beauty Meets Functionality,” Trends in Biochemical Sciences, vol. 41, pp. 261–273, 2016.
[28] J. M. Hollander, D. Thapa, and D. L. Shepherd, “Physiological and structural differences in spatially distinct subpopulations of cardiac mitochondria: influence of cardiac pathologies,” The American Journal of Physiology-Heart and Circulatory Physiology:, vol. 307, pp. H1–H14, 2014.
[29] M. Schwarzer, A. Schrepper, P. A. Amorim, M. Osterholt, and T. Doenst, “Pressure overload differentially affects respiratory capacity in interfibrillar and subsarcolemmal mitochondria,” American Journal of Physiology-Heart and Circulatory Physiology, vol. 304, pp. H529–H537, 2013.
[30] A. Riva, B. Tandler, E. J. Lesnefsky, G. Conti, F. Loffredo, E. Vazquez, and C. L. Hoppel, “Structure of cristae in cardiac mitochondria of aged rat,” Journal of Mechanisms of Ageing and Development, vol. 127, pp. 917–921, 2006.
[31] G. Asemu, K. A. O’Connell, J. W. Cox, E. R. Dabkowski, W. Xu, R. F. Ribeiro, K. C. Shekar, P. A. Hecker, S. Rastogi, H. N. Sabbah, C. L. Hoppel, and W. C. Stanley, “Enhanced resistance to permeability transition in interfibrillar cardiac mitochondria in dogs: effects of aging and long-term aldosterone infusion,” The American Journal of Physiology-Heart and Circulatory Physiologyl, vol. 304, pp. H514–H528, 2013.
[32] M. Schwarzer, A. Schrepper, P. A. Amorim, M. Osterholt, and T. Doenst, “Pressure overload differentially affects respiratory capacity in interfibrillar and subsarcolemmal mitochondria,” American Journal of Physiology-Heart and Circulatory Physiology, vol. 304, pp. H529–H537, 2013.
[33] A. P. Wojtovich, S. M. Nadtochiy, P. S. Brookes, and K. Nehrke, “Ischemic preconditioning: The role of mitochondria and aging,” Journal of Experimental Gerontology, vol. 47, pp. 1–7, 2012.
[34] O. M. de la Salud, “Boleín Observatorio Nacional de Salud,” 9 12 2013. [En línea]. Available: http://www.ins.gov.co/lineas-de-accion/ons/boletin[último acceso: 26 11 2014], 2014].
[35] L. A. Gómez and T. M. Hagena, “Age-related decline in mitochondrial bioenergetics: Does supercomplex destabilization determine lower oxidative capacity and higher superoxide production?” Journal of Seminars in Cell & Developmental Biology, vol. 23, pp. 758–767, 2012.
[36] L. C. Heather, C. A. Carr, D. J. Stuckey, S. Pope, K. J. Morten, E. E. Carter, L. M. Edwards, and K. Clarke, “Critical role of complex III in the early metabolic changesfollowing myocardialinfarction,” Cardiovascular Research, vol. 85, pp. 127–136, 2010.
[37] J. McMurray, P. Dunselman, H. Wedel, J. Cleland, and M. Lindberg, “Coenzyme Q10, Rosuvastatin, and Clinical Outcomes in Heart Failure : A Pre-Specified Substudy of CORONA (Controlled Rosuvastatin Multinational Study in Heart Failure),” Journal of the American College of Cardiology, vol. 56, pp. 1196–1204, 2010.
[38] M. Ruiz-Meana, E. Núñez, E. Miro-Casas, P. Martínez-Acedo, I. Barba, A. Rodriguez-Sinovas, J. Inserte, C. Fernandez-Sanz, V. Hernando, J. Vázquez, and D. Garcia-Dorado, “Ischemic preconditioning protects cardiomyocyte mitochondria through mechanisms independent of cytosol,” Journal of Molecular and Cellular Cardiology, vol. 68, pp. 79–88, 2014.
[39] E. Dague, G. Genet, V. Lachaize, C. Guilbeau-Frugier, J. Fauconnier, C. Mias, B. Payré, L. Chopinet, D. Alsteens, S. Kasas, C. Sever, J. Thireau, C. Heymes, B. Honton, A. Lacampagne, A. Pathak, J. Sénard, and C. Galés, “Atomic force and electron microscopic-based study of sarcolemmal surface of living cardiomyocytes unveils unexpected mitochondrial shift in heart failure,” Journal of Molecular and Cellular Cardiology, vol. 64, pp. 162–172, 2014.
[40] T. Hofer, S. Servais, A. Y. Seo, E. Marzetti, A. Hiona, S. J. Upadhyay, S. E. Wohlgemuth, and C. Leeuwenburgh, “Bioenergetics and permeability transition pore opening in heart subsarcolemmal and interfibrillar mitochondria: Effects of aging and lifelong calorie restriction,” Journal of Mechanisms of Ageing and Development, vol. 130, pp. 297–307, 2009.
[41] D. G. Nicholls and S. J. Ferguson, “Bioenergetics 3,” Elsevier Science Ltd, 2002.
[42] L. Lu, R. Su, M. Liu, Y. Zheng, and P. Zhang, “Inflammatory Heart Diseases: Causes, Symptoms, and Treatments,” Cell Biochemistry and Biophysics, vol. 72, pp. 851–855, 2015.
[43] Z. Qun, D. L. Maass, S. J. Tsai, and J. W. Horton, “Cardiac Mitochondrial Damage and Inflammation Responses in Sepsis,” Surgical Infections, vol. 8, pp. 41–54, 2007.
[44] G. Tse, J. M. Yeo, Y. W. Chan, E. T. Lai Lai, and B. P. Yan, “What Is the Arrhythmic Substrate in Viral Myocarditis? Insights from Clinical and Animal Studies,” Frontiers in Physiology, vol. 7, pp. 1–11, 2016.
[45] S. Heymans, “Inflammation and cardiac remodeling during viral myocarditis,” Ernst Schering Research Foundation Workshop, vol. 55, pp. 197–218, 2006.
[46] J. Wen and N. J. Garg, “Mitochondrial Complex III Defects Contribute to Inefficient Respiration and ATP Synthesis in the Myocardium of Trypanosoma cruzi-Infected Mice,” Antioxid Redox Signal, vol. 12, pp. 27–37, 2010.
[47] A. T. Kawaguchi, M. Sugimachi, K. Sunagawa, J. Bergsland, S. Koide, and R. Batista, “Improved Left Ventricular Contraction and Energetics in a Patient with Chagas’ Disease Undergoing Partial Left Ventriculectomy,” Journal of Cardiac Surgery, vol. 16, pp. 30–33, 2001.
[48] R. L. Deibiasi, B. A. Robinson, S. Leser, D. Brown, C. Long, and P. Clarke, “Critical Role for Death-Receptor Mediated Apoptotic Signaling in Viral Myocarditis,” Journal of Cardiac Failure, vol. 16, pp. 901–910, 2010.
[49] J. Wei, D. F. Gao, H. Wang, R. Yan, Z. Q. Liu, Z. Y. Yuan, J. Liu, and M. X. Chen, “Impairment of Myocardial Mitochondria in Viral Myocardial Disease and Its Reflective Window in Peripheral Cells,” PLos One, vol. 9, pp. 1–18, 2014.
[50] M. Guglin and L. Nallamshetty, “Myocarditis: Diagnosis and Treatment,” Current Treatment Options in Cardiovascular Medicine, vol. 14, pp. 637– 651, 2012.
[51] A. Shauer, I. Gotsman, A. Keren, D. R. Zwas, Y. Hellman, R. Durst, and D. Admon, “Acute viral myocarditis: current concepts in diagnosis and treatment,” The Israel Medicine Association Journal, vol. 15, pp. 180–185, 2013.
[52] M. H. Khandaker, R. E. Espinosa, R. A. Nishimura, L. J. Sinak, S. N. Hayes, R. M. Melduni, and J. K. Oh, “Pericardial Disease: Diagnosis and Management,” Mayo Clinic Proceedings, vol. 85, pp. 572–593, 2010.
[53] C. M. Oakley, “Myocarditis, pericarditis and other pericardial diseases,” Heart, vol. 84, pp. 449–454, 200.
[54] P. A. Kramer, B. K. Chacko, D. J. George, D. Zhi, C. C. Wei, L. J. Dell’Italia, S. J. Melby, J. F. George, and V. M. Darley-Usmar, “Decreased Bioenergetic Health Index in monocytes isolated from the pericardial fluid and blood of post-operative cardiac surgery patients,” Bioscience Reports, vol. 35, pp. 1–10, 2015.
[55] J. Soler-Soler, J. Sagristà -Sauleda, and G. Permanyer-Miralda, “Relapsing pericarditis,” Heart, vol. 90, pp. 1364–1368, 2004.
[56] S. Shinde, P. Kumar, K. Mishra, and N. Patil, “Defect in mitochondrial functions in damaged human mitral valve,” Indian Journal of Clinical Biochemistry, vol. 21, pp. 156–160, 2006.
[57] D. Pierce,B. C. Calkins,andK. Thornton,“Infectious endocarditis:diagnosis and treatment,” American Family Physician, vol. 85, pp. 981–986, 2012.
[58] A. L. Báez, M. S. Lo Presti, H. W. Rivarola, P. Pons, R. Fretes, and P. Paglini Oliva, “Trypanosoma cruzi: Cardiac mitochondrial alterations produced by different strains in the acute phase of the infection,” Experimental Parasitology, vol. 120, pp. 397–402, 2008.
[59] J. Wen, S. Gupta, Z. Guan, M. Dhiman, D. Condon, C. Lui, and N. J. Garg, “Phenyl-a-tert-butyl-nitrone and Benzonidazole Treatment Controlled the MitochondrialOxidative Stress and Evolution of Cardiomyopathy in Chronic Chagasic Rats,” Journal of the American College of Cardiology, vol. 55, pp. 2499–2508, 2010.
[60] G. Lenaz and M. L. Genova, “Functional role of mitochondrial respiratory supercomplexes,” Journal of Biochimica et Biophysica Acta, vol. 1837, pp. 427–443, 2014.
[61] R. A. Perez and J. A. Enriquez, “The function of the respiratory supercomplexes: The plasticity model,” Journal of Biochimica et Biophysica Acta, vol. 1837, pp. 444–450, 2014.
[62] Y. Chaban, E. J. Boekema, and N. V. Dudkina, “Structures of mitochondrial oxidative phosphorylation supercomplexes and mechanisms for their stabilisation,” Journal of Biochimica et Biophysica Acta, vol. 1837, pp. 418–426, 2014.
[63] G. Lenaz and M. L. Genova, “Structural and functional organization of the mitochondrial respiratory chain:A dynamic super-assembly,” The International Journal of Biochemistry & Cell Biology, vol. 41, pp. 1750–1772, 2009.
[64] E. Mileykovskaya and W. Dowhan, “Cardiolipin-dependent formation of mitochondrial respiratorysupercomplexes,” Journal of Chemistry and Physics of Lipids, vol. 179, pp. 42–48, 2014.
[65] M. Rosca, P. Minkler, and C. Hoppel, “Cardiac mitochondria in heart failure: Normal cardiolipin profile and increased threonine phosphorylation of complex IV,” Journal of Biochimica et Biophysica Acta, vol. 1807,pp. 1373–1382, 2011. 251, 252, 253
[66] J. N. Blaza, R. Serreli, A. J. Jones, K. Mohammed, and J. Hirst, “Kinetic evidence against partitioning of the ubiquinone pool and the catalytic relevance of respiratory-chain supercomplexes,” Journal of Proceedings of the National Academy of Sciences, vol. 11, pp. 15735–15740, 2014.
[67] L. A. Gómez, J. S. Monette, J. D. Chavez, C. S. Maier, and T. M. Hagen, “Supercomplexes of the mitochondrial electron transport chain decline in the aging rat heart,” Journal of Archives of Biochemistry and Biophysics, vol. 490, pp. 30–35, 2009.
[68] G. Beutner, R. A. Eliseev, and G. A. PorterJr, “Initiation of Electron Transport Chain Activity in the Embryonic Heart Coincides with the Activation of Mitochondrial Complex 1 and the Formation of Supercomplexes,” Journal of PLOS ONE, vol. 9, pp. 1–25, 2014.
[69] A. Guaras, E. Perales-Clemente, E. Calvo, R. Acín-Pérez, M. LoureiroLopez, C. Pujol, I. Martínez-Carrascoso,E. Nuñez, F. García-Marque, M. A. Rodríguez-Hernández, A. Cortés, F. Diaz, A. Pérez-Martos, and C. T. Moraes, “The CoQH2/CoQ Ratio Serves as a Sensor of Respiratory Chain Efficiency,” Journal of Cell Reports, vol. 15, pp. 197–209, 2016.
[70] G. Petrosillo, N. Di Venosa, F. M. Ruggiero, M. Pistolese, D. D’Agostino, E. Tiravanti, T. Fiore, and G. Paradies, “Mitochondrial dysfunction associated with cardiac ischemia/reperfusion can be attenuated by oxygen tension control. Role of oxygen-free radicals and cardiolipin,” Journal of Biochimica et Biophysica Acta, vol. 1710, pp. 78–86, 2005.
[71] L.Böttinger,S.E.Horvath,T.Kleinschroth,C.Hunte,G.Daum,N. Pfanner, and T. Becker, “Phosphatidylethanolamine and cardiolipin differentially affect the stability of mitochondrialrespiratorychain supercomplexes,” Journal of Molecular Biology, vol. 423, no. 5, pp. 677 – 686, 2012. [Online]. Available: http://www.sciencedirect.com/science/article/pii/S0022283612007206
[72] G. Lenaz,A. Baracca,G. Barbero,C. Bergamini,M. E. Dalmonte, M. Del Sole, M. Faccioli, A. Falasca, R. Fato, M. L. Genova, G. Sgarbi, and G. Solaini, “Mitochondrial respiratory chain super-complex I-III in physiology and pathology,” Journal of Biochimica et Biophysica Acta - Bioenergetics, vol. 1797, pp. 633–640, 2010.
[73] L. Peyta, K. Jarnouen, M. Pinault, C. Guimaraes, J. P. Pais de Barros, S. Chevalier, J. F. Dumas, F. Maillot, G. M. Hatch, P. Loyer, and S. Servais, “Reduced cardiolipin content decreases respiratory chain capacities and increases ATP synthesis yield in the human HepaRG cells,” Journal of Biochimica et Biophysica Acta, vol. 1857, pp. 443–453, 2016.
[74] L. Pokorná, P. Cermáková, A. Horváth, M. G. Baile, S. M. Claypool, P. Griac, J. Malínský, and M. Balážová, “Specific degradation of phosphatidylglycerol is necessary for proper mitochondrial morphology and function,” Biochimica et Biophysica Acta (BBA) - Bioenergetics, vol. 1857, no. 1, pp. 34 – 45, 2016. [Online]. Available: http://www.sciencedirect.com/science/article/pii/S000527281500211X
[75] R. Van Gestel, P. Rijken, S. Surinova, M. O’Flahertya, A. Hecka, A. Killian, A. Kroon, and M. Slijpera, “The influence of the acyl chain composition of cardiolipin on the stability of mitochondrial complexes; An unexpected effect of cardiolipin in a-ketoglutarate dehydrogenase and prohibitin complexes,” Journal of Proteomics, vol. 73, pp. 806–814, 2010.
[76] K. Chatfield, G. Sparagna, C. Sucharov, S. Miyamoto, J. Grudis, R. Sobus, J. Hijmans, and B. Stauffer, “Dysregulation of cardiolipin biosynthesis in pediatricheartfailure,” Journal of Molecular and Cellular Cardiology, vol.74, pp. 251–259, 2014.
[77] A. Biala, E. Tauriainen, A. Siltanen, J. Shi, S. Merasto, M. Louhelainen, E. Martonen, P. Finckenberg, D. N. Mueller, and E. Mervaala, “Resveratrol induces mitochondrial biogenesis and ameliorates Ang II-induced cardiac remodeling in transgenic rats harboring human renin and angiotensinogen genes,,” Blood Pressure, vol. 19, pp. 196–205, 2010.
[78] M. Ikeuchi, H. Matsusaka, D. Kang, S. Matsushima, T. Ide, T. Kubota, T. Fujiwara, N. Hamasaki, A. Takeshita, K. Sunagawa, and H. Tsutsui, “Over expression of Mitochondrial Transcription Factor A Ameliorates Mitochondrial Deficiencies and Cardiac Failure After Myocardial Infarction,,” Heart Failure, vol. 112, pp. 683–690, 2005.
[79] H. Sasaki,H. Asanuma, M. Fujita, H. Takahama,M. Wakeno, S. Ito, A. Ogai, J. Asakura, M. amd Kim, T. Minamino, S. Takashima, S. Sanada, M. Sugimachi, K. Komamura, N. Mochizuki, and M. Kitakaze, “Metformin Prevents Progression of Heart Failure in Dogs Role of AMP-Activated Protein Kinase,,” Heart Failure, vol. 119, pp. 2568–2577, 2009.
[80] M. Bayeva, M. Gheorghiade, and H. Ardehali, “Mitochondria as a Therapeutic Target in Heart Failure,,” Journal of the American College of Cardiology, vol. 61, pp. 599–610, 2013.
[81] K. Chandran, D. Aggarwal, R. Q. Migrino, J. Joseph, D. McAllister, E. A. Konorev, W. E. Antholine, J. Zielonka, S. Srinivasan, N. G. Avadhani, and B. Kalyanarama, “Doxorubicin inactivates myocardial cytochrome c oxidase in rats: cardioprotection by Mito-Q,,” Biophysical Journal, vol. 96, pp. 1388– 98, 2009.
[82] T. Liu, D. A. Brown, and B. O’Rourke, “Highlighted Article Role of mitochondrial dysfunction in cardiac glycoside toxicity,,” Journal of Molecular and Cellular Cardiology, vol. 49, pp. 728–736, 2010.
[83] S. A. Mortensen, F. Rosenfeldt, A. Kumar, P. Dolliner, K. J. Filipiak, D. Pella, U. Alehagen, G. Steurer, and G. P. Littarru, “The Effect of Coenzyme Q10 on Morbidity and Mortality in Chronic Heart Failure Results From QSYMBIO: A Randomized Double-Blind Trial,,” JACC: Heart Failure, vol. 2, pp. 641–9, 2014.
[84] H. N. Sabbah, R. C. Gupta, S. Kohli, M. Wang, S. Hachem, and K. Zhang, “Chronic Therapy With Elamipretide (MTP-131), a Novel MitochondriaTargeting Peptide, Improves Left Ventricular and Mitochondrial Function in Dogs With Advanced Heart Failure,,” Circulation: Heart Failure, vol. 9, p. e002206, 2016.
[85] K. Magyar, R. Halmosi, A. Palfi, G. Feher, L. Czopf, A. Fulop, I. Battyany, B. Sumegi, K. Toth, and E. Szabados, “Cardioprotection by resveratrol: A human clinical trial in patients with stable coronary artery disease,,” Clinical Hemorheology and Microcirculation, vol. 50, pp. 179–87, 2012.
[86] R. Stewart Grant, N. Braidy, G. Guillemin, and G. Smythe, “Pharmaceutical formulations of resveratrol and methods of use thereof for treating cell disorders,” New South Wales Patente WO 2009108999 A1, 2009.
[87] M. P. Murphy and R. A. Smith, “Mitochondrially Targeted Antioxidants,” Otago Patente US 6331532 B1, 2001.
[88] D. Velasco Sánchez, A. Aracil, R. Montero, A. Mas, L. Jiménez, M. O’Callaghan, M. Tondo, A. Capdevila, J. Blanch, R. Artuch, and M. Pineda, “Combined Therapy with Idebenone and Deferiprone in Patients with Friedreich’s Ataxia,” Cerebellum, vol. 10, pp. 1–8, 2011.
[89] Y. S. Sohn, W. Breuer, A. Munnich, and Z. I. Cabantchik, “Redistribution of accumulated cell iron: a modality of chelation with therapeutic implications,” Blood, vol. 111, pp. 1690–1699, 2008.
[90] A. Munnich, M. Spino, and I. Cabantchik, “Use of Deferiprone and Methods to Treat and/or Prevent Friedreich Ataxia Resulting from Intracellular Mishandling of Iron,” Patente US20130190365 A1, 2013.
[91] B. O’Rourke and T. Liu, “Methods for treating heart failure by inhibiting the mitochondrial sodium-calcium exchanger (mNCE),” US Patente US 20120077763 A1, 2012.
[92] S. J. Thandapilly, P. Wojciechowski, J. Behbahani, X. L. Louis, L. Yu, D. Juric, M. A. Kopilas, H. Anderson, and T. Netticadan, “Resveratrol Prevents the Development of Pathological Cardiac Hypertrophy and Contractile Dysfunction in the SHR Without Lowering Blood Pressure,” American Journal of Hypertension, vol. 23, pp. 192–196, 2010.
[93] D. Graham, N. N. Huynh, C. A. Hamilton, E. Beattie, R. A. Smith, H. M. Cochemé, M. P. Murphy, and A. F. Dominiczak, “Mitochondria-Targeted Antioxidant MitoQ10 Improves Endothelial Function and Attenuates Cardiac Hypertrophy,” Hypertension, vol. 54, pp. 322–328, 2009.